The BART Foundation aims to promote better outcomes for brain injury survivors by answering three questions – Which alternative therapies are likely to work, where can they be found, and how can they be afforded? One of the ways we fulfill our mission is by carefully watching global research and clinical trial outcomes and sharing that information in user-friendly language with the TBI/ABI community. While deep brain stimulation (DBS) is not one of the treatments the BART Foundation currently advocates for, it is an area worthy of attention and consideration for those with TBI/ABI.
This article appears on the Weill Cornell Medicine website, published on December 4, 2023. Please visit their webpage for the complete article. The introductory section is provided below.
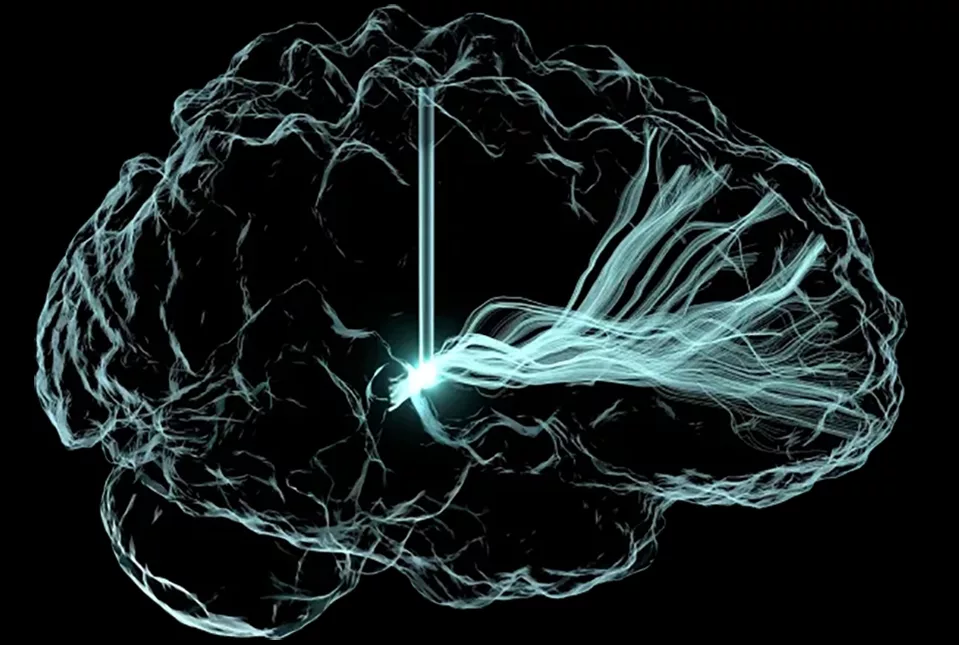
Deep Brain Stimulation Improves Cognition During Chronic Recovery Phase of Brain Injury
Five people who had life-altering, seemingly irreversible cognitive deficits following moderate to severe traumatic brain injuries showed substantial improvements in their cognition and quality of life after receiving an experimental form of deep brain stimulation (DBS) in a phase 1 clinical trial. The trial, reported Dec. 4 in Nature Medicine, was led by investigators at Weill Cornell Medicine, Stanford University, the Cleveland Clinic, Harvard Medical School and the University of Utah.
The findings pave the way for larger clinical trials of the DBS technique and offer hope that cognitive deficits associated with disability following traumatic brain injury (TBI) may be treatable, even many years after the injury.
The DBS stimulation, administered for 12 hours a day, targeted a brain region called the thalamus. After three months of treatment, all the participants scored higher on a standard test of executive function that involves mental control, with the improvements ranging from 15 to 55 percent.
The participants also markedly improved on secondary measures of attention and other executive functions. Several of the participants and their family members reported substantial quality of life gains, including improvements in the ability to work and to participate in social activities, according to a report describing participant and family perspectives from the trial. Dr. Joseph Fins, the E. William Davis, Jr., MD Professor of Medical Ethics at Weill Cornell Medicine, led that research effort.
“The ability to keep your focus and ignore the other things that aren’t important to focus on is very, very important to a lot of things in life,” one participant said in the report. “You never know what a blessing it is until you get it the second time.”
“These participants had experienced brain injury years to decades before, and it was thought that whatever recovery process was possible had already played out, so we were surprised and pleased to see how much they improved,” said study co-senior author Dr. Nicholas Schiff, the Jerold B. Katz Professor of Neurology and Neuroscience in the Feil Family Brain and Mind Research Institute at Weill Cornell Medicine.
“Our aim now is to expand this trial, to confirm the effectiveness of our DBS technique, and to see how broadly it can be applied to TBI patients with chronic cognitive deficits,” said study co-senior author Dr. Jaimie Henderson, the John and Jene Blume – Robert and Ruth Halperin Professor in the Department of Neurosurgery at Stanford University School of Medicine.
